Managing insurance billing for your ABA clinic doesn’t have to be a headache. Discover what features make the best ABA billing software — from integrated claims to real-time denial prevention — and how to choose a system that protects your bottom line.

Introduction
Insurance billing in ABA is complex, high-stakes, and time-sensitive. One error can delay reimbursement by weeks — or cost you the entire claim. That’s why choosing the best ABA billing software isn’t just a tech decision — it’s a revenue-critical strategy.
If your clinic works with Medicaid, private insurers, or managed care organizations, you need ABA billing software that’s built to handle payer rules, CPT logic, and documentation enforcement — automatically.
Why Insurance Billing Is So Risky in ABA
Even experienced billing teams struggle with:
- Denials due to expired staff credentials
- Claims rejected for improper CPT coding
- Missed billing deadlines
- Unsubmitted claims from incomplete session documentation
- Incorrect units billed outside authorization windows
These aren’t “bad luck” issues. They’re the result of missing systems. And the best ABA software prevents them by design.
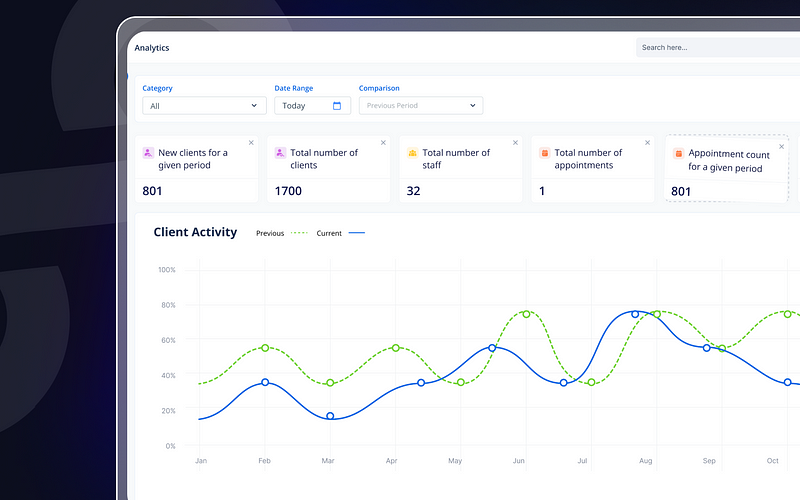
Features That Define the Best ABA Billing Software
Whether you run a solo practice or a multi-site clinic, your billing platform should include:
1. Integrated Claims Generation
Builds claims directly from session data, tied to the right CPT codes (e.g., 97153, 97155) and modifiers, minimizing manual input.
2. Real-Time Credential and Authorization Checks
Prevents claims from being generated if the session violates credential or authorization rules — reducing denials.
3. Clearinghouse Integration
Submit directly through partners like OfficeAlly or Availity, with tracking of claim status, denials, and payment timelines.
4. Copay and Client Balance Management
Invoice for remaining balances automatically, with alerts for missed or underpaid client responsibility.
5. Audit-Ready Documentation
Ensure every note, timestamp, and signature is in place before billing is allowed — streamlining compliance and protecting reimbursement.
Together, these features make ABA billing software a revenue shield — not just a payment processor.
What to Avoid in ABA Billing Software
Insurance-focused clinics should be cautious of platforms that:
- Require separate tools for documentation and claims
- Don’t enforce credential rules in scheduling
- Charge extra for basic billing features
- Lack payer-specific configuration flexibility
- Make you rely on manual claim scrubbing
In 2025, that’s not just inefficient — it’s a revenue risk.
Case Study: Slashing Denials with Smart Billing Software
A midsize ABA provider working with six insurers faced ongoing claim delays and denials due to:
- Overdue documentation
- Mismatched CPT codes
- Sessions billed by unqualified staff
After switching to a fully integrated ABA billing software platform:
- Denials dropped by 70%
- Billing turnaround time improved by 40%
- Admin staff recovered 10+ hours weekly for other tasks
The result? Consistent cash flow and confident compliance — even across complex payer mixes.
How to Evaluate the Best Software for ABA Billing
When reviewing platforms, ask:
- Can I generate and submit claims without re-entering data?
- Are credential and authorization rules checked automatically?
- Does it track client balances, denials, and payer timelines?
- Are all billing tools included — or will I need third-party add-ons?
- Does it reduce admin time while improving billing accuracy?
If the answer is “no” to any of these, it’s not the best ABA billing software for your clinic.

Conclusion
Billing is where revenue turns into reality. And in insurance-focused ABA clinics, that process must be precise, compliant, and fast.
The best ABA billing software doesn’t just send claims — it protects your revenue, prevents denials, and simplifies complexity through automation. For clinics that bill insurance, it’s not optional — it’s foundational.
FAQs
1. Do all ABA billing tools handle insurance equally?
No. Many generic systems lack payer rule enforcement, CPT configuration, or authorization logic required for clean claims.
2. Can billing software really reduce denials?
Yes. Platforms that check credentials, authorization units, and documentation status before billing eliminate common denial triggers.
3. What’s the biggest mistake clinics make with billing software?
Using separate tools for notes, credentials, and billing — which leads to data mismatches and missed compliance checks.
4. Is clearinghouse integration essential?
Absolutely. It allows direct claim submission, status tracking, and faster issue resolution.
5. How fast is ROI with good billing software?
Most clinics see ROI within the first few billing cycles, thanks to faster cash flow and fewer rejections.
