ABA billing and authorization automation is transforming how clinics prevent revenue loss and reduce admin burden. In ABA therapy , the biggest operational slowdowns often come not from delivering care, but from managing authorizations and insurance billing.
Manual tracking methods, underdeveloped software, or tools not built for ABA lead to missed units, claim denials, and delays in reimbursement. Multiply that across a growing caseload, and clinics quickly find themselves buried in rework and lost income.
Smart, built-in automation changes the game. The right platform doesn’t just record authorizations and claims – it actively enforces them, catches mistakes before they happen, and ensures every session is billable, compliant, and processed fast.
The Real Cost of Manual Billing and Authorization Workflows
Without the right system in place, ABA billing and authorization automation is missing – and workflows become constant points of failure. Most clinics don’t see the full cost until it’s too late:
- Lost revenue from expired or unverified authorizations
- Denied claims caused by incomplete documentation, wrong CPT codes, or non-matching credentials
- Unbilled units when sessions are left hanging due to scheduling or billing breakdowns
- Hours of admin time spent cross-referencing spreadsheets, claim portals, and staff credentials
Even minor errors – like submitting a claim with incomplete units – can lead to automatic rejections. And because insurance companies don’t reimburse for partial units, clinics lose money on time they’ve already delivered.
These issues don’t happen because staff are careless – they happen because the system doesn’t stop them from happening.
What Smart Automation Looks Like in an ABA Platform
Truly smart ABA billing and authorization automation means the system does the thinking for you and prevents problems from entering your workflow in the first place.
What that looks like:
- Authorization-aware scheduling
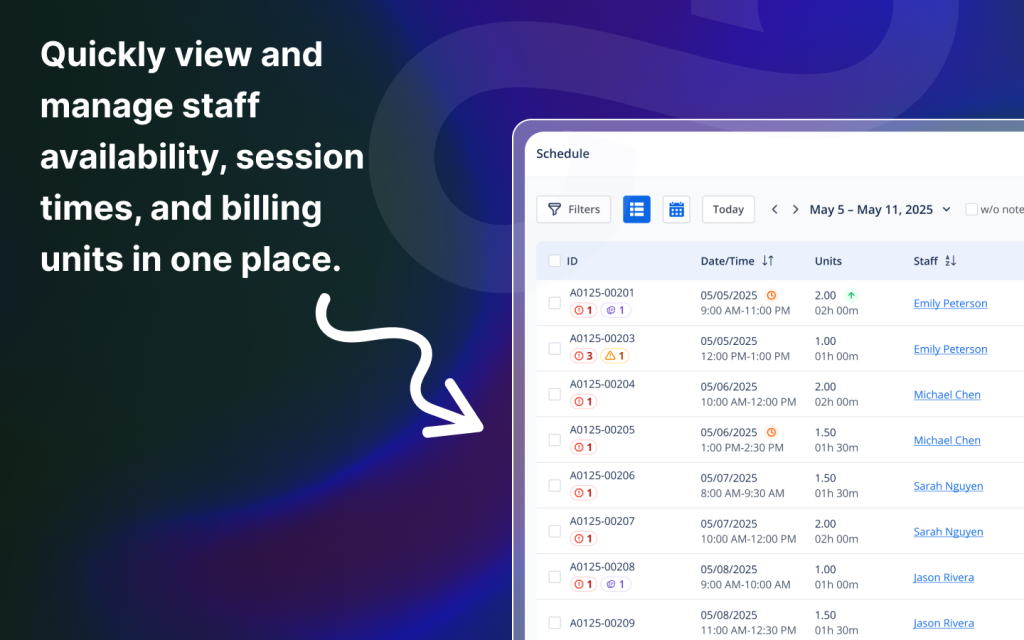
Sessions can’t be scheduled beyond authorization start/end dates or over the allowed unit total. Recurring appointments can be aligned directly to auth windows. - Real-time unit tracking
See exactly how many units have been used, reserved, or remain. Drill into individual sessions and make adjustments as needed. - Automatic claim generation
As soon as a session is completed, a claim is created. You can submit all claims in bulk via OfficeAlly, or export a universal 1500-form file for other clearinghouses. - Credential and CPT code validation
If a staff member doesn’t meet the credential requirement for a specific CPT code, the system blocks them from being scheduled or rendering services. - Pre-submission claim checks
Sessions missing required documentation – such as notes, signatures, or service alignment – can’t be billed. The system also flags incomplete units before submission to ensure no rejected claims due to partial data.
Instead of checking for errors after the fact, the software prevents them by design – saving time, protecting revenue, and streamlining the workflow for every staff member.
Tracking Authorizations Without Spreadsheets
Spreadsheets may feel familiar, but they were never designed to handle ABA billing and authorization automation needs effectively. Manually tracking units, dates, and services is time-consuming and error-prone. A smart ABA platform eliminates the guesswork and manual reconciliation.
Key capabilities to look for:
- Unit-level breakdowns
View used, reserved, and remaining units at the individual authorization level – broken down by service type (e.g., 97153, 97155). - Session-level traceability
Click into any authorization to see which specific sessions consumed units. Need to adjust or reschedule? Edit the session directly from the same view. - Start/end date filters
Align appointments with authorization windows. When scheduling recurring sessions, the system can auto-suggest dates that match the valid range. - Visual expiration warnings
Expired authorizations are flagged in red on the calendar and appointment details, helping staff avoid non-billable sessions before they happen.
This level of visibility replaces guesswork with clarity – keeping services compliant and billable without tedious admin work.

Preventing Claim Denials Before They Happen
Claim denials often trace back to a handful of repeatable errors: mismatched credentials, missing documentation, invalid CPT codes, or sessions delivered outside authorization limits.
Smart ABA software stops these errors at the source:
- Credential validation at scheduling
Staff can’t be assigned to appointments for services they’re not qualified to provide. If their TB test, DOJ clearance, or license is expired, they’re blocked. - Billing-blocking logic for incomplete sessions
If session notes or caregiver/BCBA signatures are required and not present, the system will stop the claim from being submitted. - CPT checks against payer and credential rules
CPT codes are validated against the staff’s credential and the authorization. No more mismatched submissions that lead to denials. - Alerts for expired or mismatched authorizations
Visual flags and appointment-level errors notify staff before a claim is created — ensuring every submitted claim is clean.
Prevention is better than resubmission. These automations don’t just save money – they protect staff time and client continuity.
Reducing Admin Load with Built-in Billing Automation
ABA billing is a full-time job – unless your system does the heavy lifting. With smart automation, clinics can process more claims, faster, with fewer errors and less staff overhead.
Here’s what that looks like:
- Auto-generation of claims upon session completion
No need to manually enter service codes or session data – everything flows from the appointment. - Bulk claim submission
Clinics can submit multiple claims through OfficeAlly in one click, or export a single file containing 1500-forms ready for upload to any clearinghouse. - Aging and claim status visibility
Track which claims are pending, denied, or paid. Use aging filters to follow up before revenue is delayed or lost. - Automatic invoicing for client responsibility
As payments are posted, the system automatically generates invoices for remaining balances like copays and coinsurance. These can be paid directly online or printed for mailing.
The result is a billing workflow that scales with your clinic – without scaling your admin team.

How Payer-Specific Invoicing Helps You Get Paid Faster
Getting reimbursed isn’t just about submitting claims – it’s about submitting them in the format your payers want. Mismatched invoice structures, missing data fields, and unapproved formats can lead to delays or outright rejections.
The right system handles that for you:
- Payer-specific templates
Invoices and claims are generated in the layout and format required by each insurance provider. - Separation of financial responsibilities
Automatically generate separate invoices for client copay, coinsurance, or private pay obligations after payer payments are posted. - Built-in reconciliation tools
Match posted payments to claims, track balances, and monitor aging reports to follow up on unpaid claims quickly and accurately. - One-click claim packaging
Whether you’re submitting via OfficeAlly or another clearinghouse, batch and send claims in seconds, reducing turnaround time.
Invoicing becomes a process you trust, not a process you chase.
Real-World Impact: Before and After Smart Billing Tools
Let’s look at the difference these tools make in practice.
A mid-sized ABA clinic used to manage authorizations in spreadsheets and process claims manually. Staff spent 15–20 hours per week on billing-related rework, often chasing denials from sessions that fell outside authorization limits or were missing credentials.
After switching to a system with embedded billing and authorization controls:
- Claim rejections dropped by 60%
- Time spent on reprocessing or resubmissions was cut in half
- Revenue was recovered faster thanks to automatic tracking and alerts
- Admin staff were able to shift from data entry to client support
The software didn’t just streamline billing – it reshaped the entire operational rhythm of the clinic.
Conclusion
ABA clinics lose more time and money to operational blind spots than they realize. Authorization errors, incomplete claims, mismatched credentials, and outdated billing workflows chip away at margins and morale.
The solution isn’t more admin – it’s smarter automation.
The best ABA platforms enforce authorization rules, validate credentials in real time, track unit usage, and automate claims end to end – so your team can focus on care, not compliance.
TherapyLake is built with those exact principles: no contracts, no onboarding fees, no gimmicks – just operationally smart software for ABA clinics. With a free trial, flat pricing, and payer-tested workflows, it’s the platform that removes billing friction from the ground up.
FAQs
1. How does ABA software track authorization units?
Units are displayed in real time – used, reserved, and remaining – broken down by service code. Clinics can click in to view which sessions used specific units.
2. Can I schedule appointments based on authorization windows?
Yes. The system prevents scheduling outside of auth start/end dates and can align recurring sessions automatically.
3. What happens if a session is submitted without proper documentation?
Claims are blocked from submission until all required notes and signatures are attached – ensuring no rejected or incomplete claims.
4. How do billing tools handle payer-specific claim logic?
Each claim or invoice is formatted according to payer-specific requirements to prevent rejections and speed up reimbursements.
5. Is it possible to avoid denials entirely with automation?
While no system can prevent every payer issue, platforms like TherapyLake significantly reduce denials by enforcing rules before claims are submitted.
