In 2025, efficient ABA practice management isn’t just about reducing hours or staff burnout – it’s about letting your systems do the heavy lifting. With rising caseloads, tighter payer requirements, and growing staffing needs, ABA clinics need tools that operate like silent partners: enforcing rules, automating workflows, and eliminating admin friction.
This blog explores what efficient ABA practice management really means today, and how the smartest clinics are doing more with less – without compromising care, compliance, or revenue.

Why ABA Clinics Still Struggle with Efficient ABA Practice Management
Even with modern software, many ABA clinics are stuck doing work their systems should be automating. Common pain points include:
- Manual credential tracking via spreadsheets
- Billing errors from mismatched CPT codes or expired staff licenses
- Authorizations not enforced, leading to denials
- Scheduling overload from tools that don’t check for conflicts or expirations
- Rework and resubmissions due to incomplete documentation
What’s the root cause? Tools not built for ABA – or systems that require staff to remember compliance instead of enforcing it by design.
What Makes ABA Practice Management “Efficient”?
Efficiency isn’t just a feature set – it’s an outcome. Efficient ABA practice management software:
- Reduces manual work
- Prevents errors before they happen
- Scales without increasing headcount
- Improves revenue cycle without extra overhead
The key? Built-in logic that governs every step – so the system becomes your first line of defense against administrative drag.
Core Features of Efficient ABA Practice Management Software
Here are the components every ABA clinic should expect from efficient practice management tools in 2025:
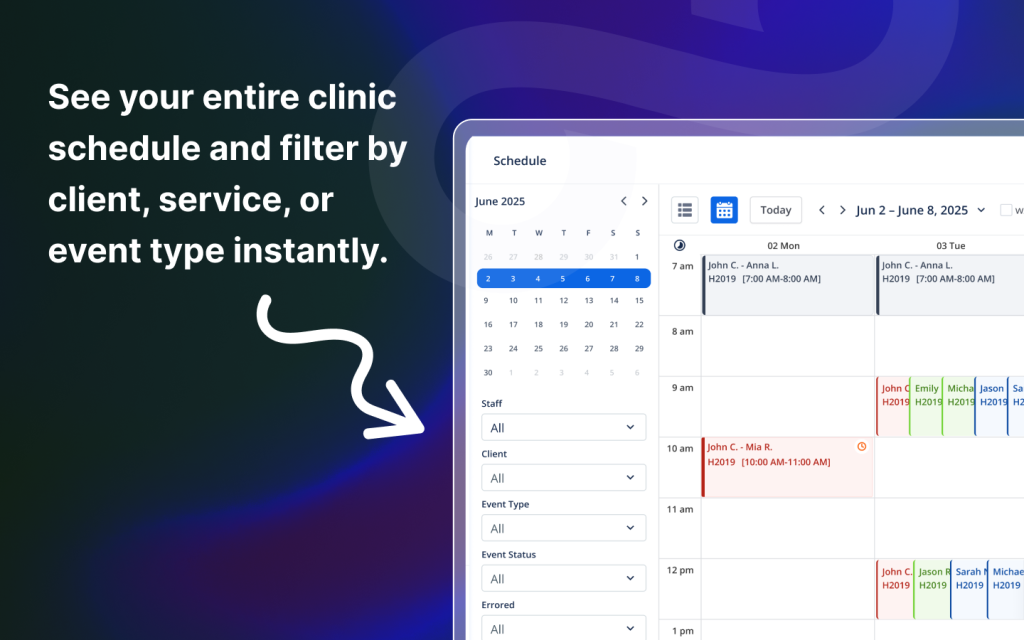
- Credential-Aware Scheduling
Blocks expired or unqualified staff from being assigned. Enforces TB test, DOJ, CPR, and license requirements in real time. - Authorization-Based Appointment Rules
Limits sessions to the start/end dates and unit caps defined by payers. Aligns recurring appointments with valid auth windows automatically. - Real-Time Billing Automation
Claims are generated from completed sessions with all required data — then submitted through clearinghouses with just one click. - Pre-Billing Compliance Checks
Generates claims from completed sessions with all required data, then submits them through clearinghouses with just one click. - Session-Level Audit Trails
Every session includes time-stamped notes, e-signatures, and credential verification to support clean claims and payer audits. - Role-Based Dashboards
Admins, schedulers, and clinicians see only what they need – reducing clutter and mistake risks.
These tools don’t just help you do more – they make sure every task is done right the first time.
Scaling Without Sacrificing Efficiency
Most clinics lose efficiency as they grow – because they add tools, not automation.
With the right platform, your team should be able to:
- Add staff without new spreadsheets or training overhead
- Schedule 100+ sessions per week without calendar chaos
- Submit 5x more claims without increasing billing headcount
- Stay compliant with less effort, not more micromanagement
Case Study: How Efficient ABA Practice Management Replaces Admin Rework
A growing ABA clinic with 60 clients and 15 staff struggled with:
- Missed units due to expired authorizations
- Claims held up due to incorrect CPT codes
- Credential expirations going unnoticed
After adopting an all-in-one ABA platform with built-in billing and compliance logic:
- Weekly claim submission time dropped from 8 hours to under 2
- Credential mismatches were reduced to zero
- Admin time was redirected toward onboarding and client service – not fixing errors
The result: smoother operations, happier staff, and more billable sessions.

How to Measure Efficiency in ABA Software
When evaluating ABA practice management software, consider these questions:
- Does the system prevent compliance issues – or just report them?
- Are workflows streamlined across scheduling, billing, and documentation?
- Can your staff focus on care instead of chasing paperwork?
- Will the platform adapt as your client base grows?
If your software isn’t saving you hours or reducing risk, it’s not efficient – it’s just a digital version of your old problems.
Conclusion
Efficient ABA practice management in 2025 isn’t about cutting staff or doing more tasks – it’s about empowering your team with systems that enforce best practices, prevent revenue loss, and reduce operational headaches.
If your current platform isn’t doing that, it may be time to consider one that is.
FAQs
1. What’s the biggest barrier to efficiency in ABA clinics?
Manual systems and generic tools that don’t understand ABA workflows – especially for credentialing and billing.
2. Can efficient systems really reduce staff workload?
Yes. Automation cuts rework, prevents claim denials, and minimizes compliance errors, freeing your team for higher-value tasks.
3. Do efficient systems cost more?
Not necessarily. The right platform pays for itself in time saved, claims recovered, and admin hires avoided.
4. Is automation risky for compliance?
Not when it’s ABA-specific. Smart platforms use guardrails to enforce payer and credential rules.
5. How do I know if my current system is inefficient?
If your staff are cross-checking spreadsheets, fixing denials, or manually enforcing credentials – it’s time for an upgrade.

Casinolebull, eh? I’ve seen worse. The games selection is alright and the sign up bonus is relatively decent. Worth a punt if you’re bored. Find it here: casinolebull
Bet364games… not sure if it’s connected to the bigger brand, but it does what it says on the tin. Games are alright, not amazing, but worth checking out if you’re after some quick spins. Check it here: bet364games
Richi777casino has a classic, slightly old-school feel. But the games are there, and if you’re into jackpot hunts, this might be your cup of tea. Decent range too. Go check it: richi777casino